Diagnosis
Although spinal pain is usually the first and most common symptom of axial spondyloarthritis (axSpA), individuals with axSpA may also experience pain, stiffness, and limited mobility in the hips, knees, heels, and other joints. Notably, lower back pain can only be clinically defined—that is, it cannot be defined by laboratory tests such as C-reactive protein (CRP) or erythrocyte sedimentation rate (ESR)—making it difficult to establish the underlying cause.1
The hallmark feature of axSpA is inflammatory back pain. Inflammatory back pain in patients with axSpA usually presents with the following general characteristics2:
- Occurs in early adulthood (before 45 years of age)
- Gradual onset
- Lasts longer than 3 months
- Improvement of pain with exercise but not rest
- Wakes patient up in the second half of the night
- Associated with morning stiffness lasting more than 30 minutes
- May be associated with buttock pain that alternates between the left and right sides
- Occurs in early adulthood (before 45 years of age)
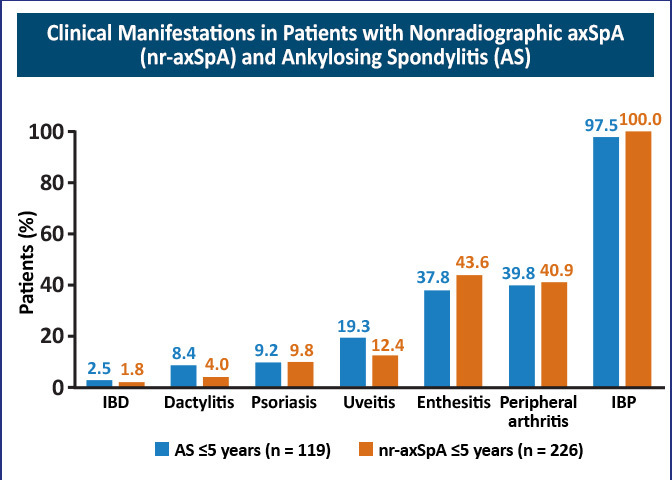
Although axSpA is predominantly a disease of the axial skeleton, it frequently affects peripheral joints and extraarticular organs. Common features of spondyloarthritis include peripheral inflammatory arthritis, enthesitis, uveitis, dactylitis, psoriasis, Crohn’s disease or ulcerative colitis, a family history of spondyloarthritis, human leukocyte antigen B27 (HLA-B27) positivity, and elevated CRP.2
Figure 1: Clinical Manifestations in Patients With Nonradiographic AxSpA (nr-axSpA) and Ankylosing Spondylitis (AS)3
Referral Strategies for Nonrheumatology Providers
The average delay between symptom onset and diagnosis of axSpA is estimated to be between 5 and 14 years in the United States.2,4 Several factors contribute to the delay in diagnosis, including the high prevalence of back pain in the general population and the lack of disease awareness by nonrheumatology providers.2
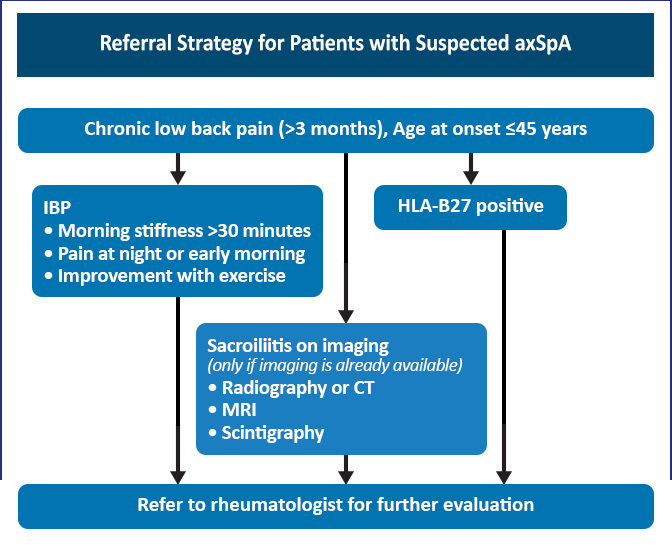
AxSpA can easily be missed in a primary care setting since no specific physical examination findings or diagnostic tests can be used to differentiate axSpA from other causes of chronic back pain. To reduce diagnostic delay, a simple referral strategy has been suggested for patients with suspected axSpA. Patients with back pain for 3 months or longer and an age of onset younger than 45 years should be screened for axSpA. The presence of inflammatory back pain, sacroiliitis on imaging, or HLA-B27 positivity in these at-risk patients should prompt referral to a rheumatologist for a possible diagnosis of axSpA.2
Figure 2: Referral Strategy for Patients With Suspected AxSpA2
Early diagnosis of axSpA is crucial to minimize disease burden. Disease activity, patient-reported pain, and impairment to quality of life are high in the early stages of disease, independent of radiographic changes.4, 5 Underrecognition of axSpA results in a missed or late diagnosis, leading to prolonged pain, stiffness, fatigue, and decreased mobility.
Early treatment of nonradiographic and radiographic axSpA improves symptoms, function, and inflammation as viewed by magnetic resonance imaging (MRI) and may prevent irreversible changes.5, 6 If left unmanaged, chronic inflammation in the sacroiliac joint and spine over time can lead to pathologic bone formation, structural damage, and, ultimately, fusion of the sacroiliac joint and spine in some patients.2 This progression can lead to several clinical and quality of life challenges such as reduced range of motion, higher risk of fracture, spinal curvature, stiff rib cage, and even breathing restrictions.7
Longer delays in diagnosis are associated with greater radiographic progression, worse spinal mobility, less favorable response to treatment, reduced quality of life, and increased direct and indirect health costs.4, 5, 6
When axSpA is initially suspected, patients should be given a prescription for an NSAID as an interim first-line treatment while a rheumatology consult is arranged. Early initiation of physical therapy is also recommended. The decision to initiate biologic therapy should be deferred to a rheumatologist following confirmation of the diagnosis and assessment of the risks and benefits of therapy.2
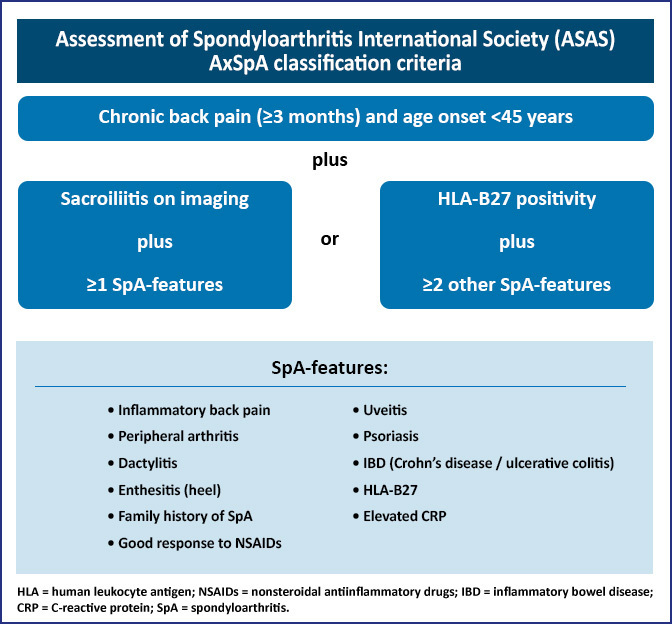
In general, the diagnosis of axSpA is a clinical judgment based on features that are characteristic of the disease. These features include a combination of historical manifestations, physical findings, laboratory results, and imaging data. Patients with suspected axSpA must be assessed carefully. Figure 3 lists the classification, but not diagnostic, criteria of axSpA.4
Figure 3: AxSpA Classification Criteria8, 9
References
- Braun J. Axial spondyloarthritis including ankylosing spondylitis. Rheumatology (Oxford). 2018;57(suppl 6):vi1-vi3.
- Magrey MN, Danve AS, Ermann J, et al. Recognizing axial spondyloarthritis: a guide for primary care. Mayo Clin Proc. 2020;95:2499-2508.
- Deodhar AA. Understanding axial spondyloarthritis: a primer for managed care. Am J Manag Care. 2019;25:S319-S330.
- Walsh JA, Magrey M. Clinical manifestations and diagnosis of axial spondyloarthritis. J Clin Rheumatol. 2021;27:e547-e560.
- Danve A, Deodhar A. Axial spondyloarthritis in the USA: diagnostic challenges and missed opportunities. Clin Rheumatol. 2019;38:625-634.
- Yi E, Ahuja A, Rajput T, et al. Clinical, economic, and humanistic burden associated with delayed diagnosis of axial spondyloarthritis: a systemic review. Rheumatol Ther. 2020;7:65-87.
- Yu D, et al. Patient education: axial spondyloarthritis, including ankylosing spondylitis (Beyond the Basics). UpToDate. 2019. https://www.uptodate.com/contents/axial-spondyloarthritis-including-ankylosing-spondylitis-beyond-the-basics/print
- Rudwaleit M, van der Heijde D, Landewe R, et al. The development of Assessment of SpondyloArthritis international Society classification criteria for axial spondyloarthritis (part II): validate and final selection. Ann Rheum Dis. 2009;68:777-783.
- Spondylitis Association of America (SAA). Overview of types of spondylitis. https://spondylitis.org/about-spondylitis/types-of-spondylitis/